No, Endurance Exercise Won’t Kill You
The heart remodels in response to intense training. Are the changes worrisome or benign?
Athens, Greece
September 12, 490 b.c.
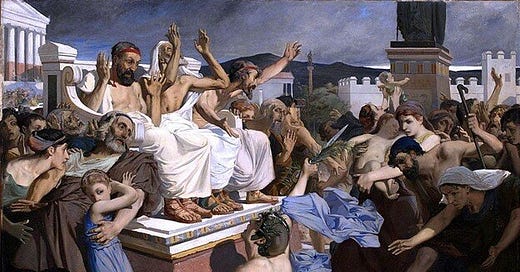
This is the site of the first known fatality related to endurance running. Upon arrival to Athens, running the now-revered distance of 26 miles to deliver a message of a military victory against the Persians, Pheidippides, our Greek hero, collapsed, most likely due to sheer exhaustion on behalf of his previous effort.
“Joy to you, we’ve won” he said, and there and then he died, breathing his last breath with the words “Joy to you.”
While an awe-inspiring anecdote, our knowledge of human limits, physiology, and the sheer number of participation in endurance sports prevents us from concluding that, directly or indirectly, running a marathon will kill you, just like it did to Pheidippides. Pheidippides’ story is provocative. Perhaps it tells a tale of what the human spirit can accomplish if truly pushed to the limits (although I don’t suggest exerting yourself to the point of death). Far from a warning for everyone to avoid running, this tale has created a “lust” around the modern 26.2 mile distance — Pheidippides lives on as hordes of runners, in one way or another, try to recreate his heroic effort each weekend.
Indeed, U.S marathon running, and endurance sport participation in general, has hit a revival. This is supported by the nearly 507,000 marathon finishers in 2016. These numbers indicate rising participation, an increase in people involved in chronic endurance exercise training for the sake of competition and health.
Is there a downside to this participation? Opponents of endurance running like to cite the infrequent cases of modern-day Pheidippides as reasons as to why endurance running is dangerous. Indeed, a “comprehensive” list of marathon-related deaths on Wikipedia contains 47 cases of “death by marathon” in the U.S and elsewhere, up until 2016.
A list of the causes of death in these marathons reveals an underlying pattern. Many, but not all, are cardiac-related issues (i.e. heart attack, arrhythmia, underlying congenital heart abnormality). We know exercise, and especially a marathon, stresses the heart, among other systems. A list like this leads one to propose that endurance running may in fact be detrimental to the cardiovascular system— it must be, to have resulted in these deaths?
However, these 47 deaths were over the span of some 35 years, over which some 4 million + people finished a marathon. What this amounts to is around 0.9–1.6 deaths/100,000 marathon finishers. Marathon running is far from a potent risk factor for an acute cardiovascular event, as evidence by the statistics.
While it is undeniable that lack of preparation, underlying cardiac issue, or freak accident may make one susceptible to irreversible injury or death, we cannot ignore the facts— very few people on a population wide level suffer from life-threatening incidents after endurance exercise or related activities.
However, provocative findings such as the ones cited above compel us to at least investigate potential mechanisms as to why endurance activity participation may be detrimental in the short term as well as when participated in over a long timespan.
Indeed, another argument against high intensity long-term endurance training is that it may actually lead to unfavorable adaptations such as the athlete’s heart (discussed later). Even adaptations such as this have been shown to be primarily physiological rather than pathophysiological in nature. The central question becomes not “is exercise good for us?” — we know that this answer is a resounding yes. However, “is more better?” has become a topic of discussion in terms of cardiovascular disease prevention and enhancement of lifespan and healthspan. Do the adverse effects of endurance exercise outweigh the benefits if one fails to abide by the law of “everything in moderation?”
Does exercise pose an acute cardiovascular risk?
As mentioned previously, a large amount of endurance sport-related deaths occurred due to a cardiac incident during or following a bout of activity. Indeed, vigorous exercise is known to increase the risk (in the near-term) of sudden cardiac death. However, it is noted that this increased risk manifests only in individuals with an underlying cardiac disease.
For instance, younger (<30 or 40 years of age) individuals who suffer from sudden cardiac death during exercise are usually found to have an inherited or congenital cardiac condition, also known collectively as cardiomyopathies. 44% of deaths among athletes in the U.S were shown to be due to hypertrophic cardiomyopathy — an inherited heart condition in which the heart is enlarged. In older adults, reasons for death often include further cardiovascular issues such as coronary artery disease. These conditions make one susceptible to risk of injury or death during high exertion activity, and prohibits drawing the same conclusions about health effects of exercise in asymptomatic individuals.
One study examining the risk of sudden cardiac death in male physicians (a “healthy” cohort) concluded that, while the risk of death was 16.9% higher during vigorous vs. lower intensity exercise, the absolute risk was still extremely low — 1 death per 1.42 million hours of vigorous exercise.
We do have evidence that one’s risk of suffering from a cardiac incident during exercise goes DOWN as you get fitter, and this makes intuitive sense. Running a marathon or vigorous endurance race when one is ill-prepared would seem to increase one’s susceptibility to injury or death. Observations support this.
When comparing the risk of death during exercise to the amount of baseline physical activity individuals participated in, risk dropped with increasing levels of activity. Additionally, among a study of 84,888 women, those who exercise 2 or more hours per week were shown to have a decreased risk of suffering an exercise-related cardiac event. In the long term, exercise thus seems to be protective in terms of health as well as for lowering one’s risk for sudden cardiac death during exercise.
Why does exercise increase the risk of a cardiac event? While I won’t touch on mechanisms, it deserves a word here to note that vigorous exercise does place quite the demand on the heart. While our hearts are robust, an underlying substrate of cardiac disease or arrhythmia may be the straw that breaks the camel’s back, so to speak.
Lower cardiac function (i.e. due to cardiac fatigue, which only occur after ultra-long duration exercise) may be one way in which one’s risk for injury rises during or after exercise. As we activate our sympathetic nervous system and release epinephrine and norepinephrine into our systems (the “fight and flight” response), heart rate and the force of the heart contraction (known as contractility) both increase. It is proposed that, over a long-term exercise bout, our body, in particular the heart, may be unable to handle the increased physical demands and may reduce its function over time. Not to worry — unless your exercise routinely lasts >3 hours many of these detrimental processes are unlikely to take place.1
Evidence tells us that the risk of an exercise-related event, among healthy individuals who regularly participate in exercise, is extremely low. Even among individuals with underlying heart conditions or CVD, vigorous exercise doesn’t seem to pose any substantial threat.
Long term exercise training and the heart: are the adaptations detrimental or beneficial?
Most of the argument over whether long-term endurance training is harmful centers around a concept referred to as the “athlete’s heart”.2 In short, the athletes heart refers to adaptations of the heart including mild to moderate enlargement of the ventricles and the heart walls, enhanced left ventricle filling, enhanced heart mechanics (twisting and untwisting during contraction), and enlargement of the atria.
In contrast to the negative left ventricular hypertrophy that is characteristic of many cardiovascular disease conditions (characterized by a thicker left ventricle wall, but a ventricle that “shrinks” causing the heart to under-perform) — the eccentric hypertrophy that occurs with training has been referred to as a positive adaptation, allowing more blood to be filled and then ejected from the ventricle. This allows for more blood delivery during exercise.
Keep reading with a 7-day free trial
Subscribe to Physiologically Speaking to keep reading this post and get 7 days of free access to the full post archives.