Physiology Friday #229: Stress Reduction Explains Why Exercise Lowers Cardiovascular Disease Risk
Is the brain the "missing link" between physical activity and heart health?
Greetings!
Welcome to the Physiology Friday newsletter.
Details about the sponsors of this newsletter including Examine.com and my book “VO2 Max Essentials” can be found at the end of the post!
“The heart never takes the place of the head: but it can, and should, obey it.”
― C.S. Lewis, The Abolition of Man
Exercise is an anti-depressant.
In fact, some studies show that exercise is better than antidepressants. Plus it makes you fitter (which antidepressants definitely don’t do).
And, at least subjectively, exercise boosts mood (ever heard of the “runner’s high”?) and relieves stress and anxiety. I never feel more at peace than after an intense run, and I’m sure you’ve experienced something similar during or after completing your preferred physical activity of choice. There’s a unique Zen-like state that comes from a workout well done.
Exercise doesn’t just make our brains feel better, it objectively makes us healthier, and one of the biggest areas of health that improves with exercise is cardiovascular health. There is no doubt about it — people who exercise have healthier hearts. Aerobic and resistance exercise both reduce cardiovascular morbidity (your risk of developing a cardiovascular disease or CVD) and mortality (your risk of dying from a CVD).
There are several distinct mechanisms to explain why exercise benefits brain health and cardiovascular health separately. Those mechanisms are well beyond the scope of this post.
But stress begins in the brain. And we know that stress — both psychological and physiological — is a risk factor for CVD. Stress harms the heart. Overactivation of the sympathetic nervous system (the “fight and flight” branch of the autonomic nervous system) elevates blood pressure, spikes heart rate, and when chronically activated, leads to low-grade inflammation. This is a recipe for CVD development.
This leads to the logical question: Could psychological stress reduction explain why exercise is so good for heart health? And what are the implications of this for people with depression who may be at a greater cardiovascular risk?
These two questions were investigated in a recent study published in the Journal of the American College of Cardiology.1
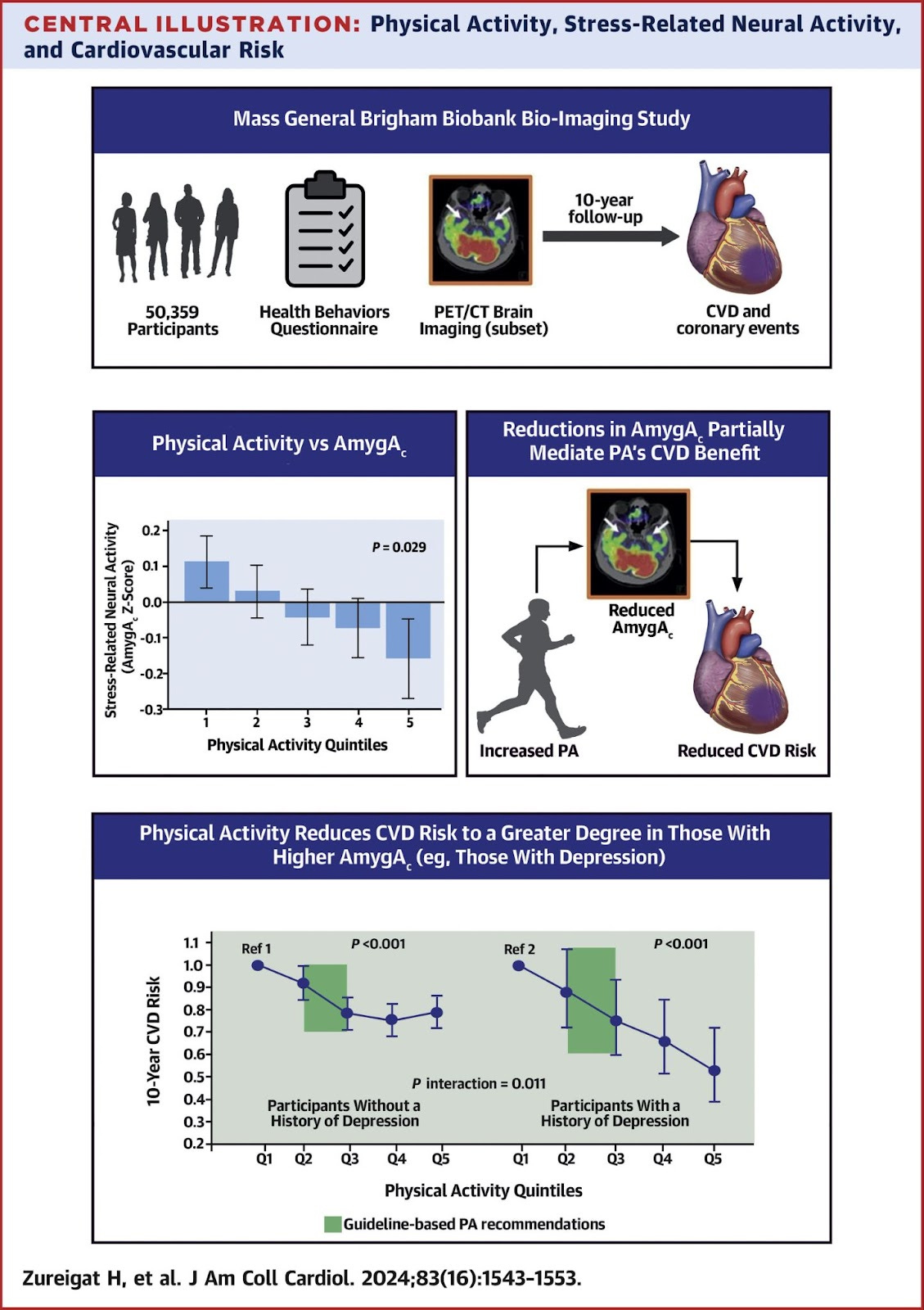
To investigate the mechanisms responsible for the CVD-reducing effects of physical activity, researchers used data from the Mass General Brigham Biobank — an electronic health data repository of more than 50,000 adults — to probe the associations between exercise, brain health, and heart health.
A total of 50,359 participants (average age of 60 and 40% male) were analyzed for the study. A subset of 744 participants with complete information on health behaviors, physical activity, genetic data, and brain metabolic activity (obtained from a brain imaging study) were included in a brain imaging substudy to investigate the neural correlates of physical activity’s cardiovascular benefits.
The brain imaging substudy involved the participants undergoing a test to measure stress-related brain activity. Specifically, they underwent 18F-fluorodeoxyglucose positron emission tomography/computed tomography (18F-FDG-PET/CT), which provides a measure of stress-related neural activity based on a ratio of metabolic activity in two brain regions: the amygdala and the ventromedial prefrontal cortex (vmPFC). The former (the amygdala) is largely activated in response to threat detection, while the latter (vmPFC) has an inhibitory function on stress-activated brain structures. Higher amygdala activity = more stress. Higher vmPFC activity = less stress. To oversimplify things.
Here’s the brain imaging procedure in more detail. For those less inclined, you can skip to the next paragraph.
18F-FDG-PET/CT is an advanced imaging technique combining two types of scans: PET (Positron Emission Tomography) and CT (Computed Tomography). In this procedure, a radioactive sugar called 18F-FDG (Fluorodeoxyglucose) is injected into the brain. Cells absorb this modified sugar similarly to regular sugar. The PET scan detects the radiation emitted by the sugar, showing how tissues and organs are functioning, while the CT scan provides detailed images of their structure. By combining these scans, researchers/healthcare professionals can get a comprehensive view of both the anatomy and metabolic activity within the body and, in this case, the brain.
In short, any change in the activation or the ratio of metabolic activity of these two brain structures — indicated by more or less 18FDG uptake — is indicative of altered stress-related behaviors and conditions, for example, anxiety, PTSD, and depression.
In the context of this study, a lower amygdala: vmPFC activity (on the left in the image below) is indicative of lower stress-related neural activity, while higher amygdala: vmPFC activity is indicates of higher stress-related neural activity (on the right in the image below).
The researchers also used the brain imaging procedure to measure atherosclerotic activity, including coronary artery calcium and arterial glucose uptake, and bone marrow and spleen white blood cell producing (leukopoietic) activity.
Using information on the participants’ self-reported levels of physical activity, the researchers then analyzed the relationships between habitual physical activity levels, brain activity, and cardiovascular disease development over a 10-year follow-up period.
Importantly, the analysis of the relationship between physical activity and stress was adjusted for confounders including age, sex, socioeconomic status, lifestyle risk factors, genetic risk scores, and medical comorbidities. Here’s what the research found.
Participants who met the minimum recommended weekly physical activity level — 150 minutes per week of moderate to vigorous exercise — had lower stress-related neural activity compared to participants who did not meet the physical activity recommendations.
There was also a dose-dependent reduction in stress-related neural activity with increasing levels of physical activity. When the participants were separated into quintiles of physical activity, those in the lowest fifth (quintile 1) had the highest level of stress-related neural activity while those in the highest fifth (quintile 5) had the lowest. Quintiles 2, 3, and 4 fell somewhere in between.
For reference, participants in quintile 1 and 2 engaged in less than 150 minutes of exercise each week (i.e., they fell below the guidelines), quintiles 3 and 4 engaged in somewhere between 5 to 10 hours of exercise per week, and quintile 5 engaged in around 10–15 hours of exercise per week.
The reduction in stress-related neural activity was driven by enhanced activity in the vmPFC (the brain region associated with inhibiting the fear response) rather than a reduction in activity of the amygdala (though there was a nonsignificant association between physical activity and lower activity in this area).
Perhaps not surprisingly, meeting the physical activity guidelines was associated with a 20% reduction in the risk of having a cardiovascular event over a 10-year follow-up period.
Greater stress-related neural activity, on the other hand, was associated with a 20% increase in the risk for CVD events and higher levels of coronary artery calcium, the inflammatory marker C-reactive protein, and white blood cell and neutrophil levels. Bone marrow and spleen leukopoietic activity was also elevated in participants with higher stress-related neural activity. In short, the more stress-related neural activity someone had, the greater their cardiovascular risk profile.
The researchers next looked at whether stress-related neural activity mediated the benefits of physical activity on cardiovascular health — and that’s exactly what they found.
There was sufficient evidence to support the pathway of increased physical activity leading to lower stress-related neural activity (AmygAc) leading to a reduction in CVD events. Specifically, about 8% of the CVD-reducing benefits of physical activity were explained by its effects on stress activity in the brain.
Because individuals diagnosed with depression have higher levels of stress-related neural activity, it follows that they might receive a greater benefit from physical activity than people without depression.
Among the adults in the study cohort with depression, physical activity was associated with a 14% lower risk of 10-year CVD events. The CVD risk reduction for most of the outcomes of interest was almost twice as high among the participants with depression than those without, indicating that adults with depression may benefit more from physical activity.
Furthermore, there appeared to be no upper limit for the benefits of physical activity on CVD risk reduction for the participants with depression, but for participants without depression, physical activity benefits plateaued after about 300 minutes of moderate to vigorous physical activity per week.
The findings of this study carry some important implications whether you have depression or not. They implicate the brain as an important factor in the cardiovascular benefits of exercise. This isn’t something that’s often talked about but that needs to be recognized!
The cardioprotective benefits of exercise are often attributed to improved endothelial function, a reduction in risk factors like cholesterol or blood glucose, and a lowering of blood pressure. But as this study shows, reduced sympathetic nervous system activity (stress-related neural activity) accounts for almost 10% of the risk reduction associated with getting enough exercise. That’s powerful stuff! (It also suggests that we really need to modify our understanding of the pathways mediating the cardiovascular benefits of exercise…see below).
This study also offers an alternative explanation for why exercise might make us “feel good.”
The so-called “runner’s high” is explained by endorphins and endocannabinoids (our body’s natural cannabis) that rush through us during and after exercise, leading to feelings of euphoria.
But what if we feel good after exercise not because we’re riding a high, but because our brain’s defense mechanisms are temporarily shut down, our stress responses quelled? This more accurately represents my personal experience with exercise. I’m less often euphoric and ecstatic after a workout. Rather, the postexercise period is a mellow, satisfied, and content experience. Rather than thank the endorphin rush, perhaps I should be thanking my ventromedial prefrontal cortex.
We like to think of the brain and body as separate entities, but that couldn’t be further from the truth. Our thoughts and our neural activity (which our thoughts are after all) are reflected in our physiology, and vice-versa.
So the next time you head out for a run or crush a few sets in the gym, remember that you are improving your cardiovascular health, and you can thank your brain for some of that.
Thanks for reading. See you next Friday.
~Brady~
The VO2 Max Essentials eBook is your comprehensive guide to aerobic fitness, how to improve it, and its importance for health, performance, and longevity. Get your copy today and use code SUBSTACK20 at checkout for a 20% discount. You can also grab the Kindle eBook, paperback, or hardcover version on Amazon.
Examine.com: Examine is the largest database of nutrition and supplement information on the internet.