Physiology Friday #230: Cutting Sugar vs. Cutting Carbs for Cardiometabolic Health
Is the ketogenic diet as sweet as it sounds?
Greetings!
Welcome to the Physiology Friday newsletter.
Details about the sponsors of this newsletter including Examine.com and my book “VO2 Max Essentials” can be found at the end of the post!
The debate over whether carbohydrates or sugar are the true culprits behind modern health issues has long stirred controversy among nutrition experts, diet enthusiasts, and the general public alike.
On one side, advocates of low-carbohydrate diets argue that cutting carbs, particularly in the form of sugars, is essential for weight management and metabolic health — pointing the rise of insulin resistance, obesity, and type 2 diabetes as evidence that our carbohydrate-laden diets are wreaking havoc on our bodies.
The other side cautions against demonizing all carbohydrates, emphasizing that not all carbs are created equal. They argue that complex carbohydrates, found in whole grains, fruits, and vegetables, are fundamental to a balanced diet, providing essential nutrients and sustained energy (and they taste good).
The crux of the issue lies in differentiating between types of carbohydrates and understanding their distinct effects on the body. Again — not all carbs are created equal.
Simple sugars, particularly those added to foods or concentrated in products like fruit juices and syrups, have been linked to spikes in blood sugar, increased fat storage, and higher overall energy intake because they promote overeating. This has led to widespread recommendations to drastically reduce "free sugars" in the diet. However, the conversation becomes more nuanced when considering carbohydrates as a broader category. Some argue that a focus on reducing overall carbohydrate intake — a low-carbohydrate or ketogenic diet — may offer benefits beyond just sugar restriction, potentially improving metabolic flexibility and reducing inflammation, among other effects.
Yet, others raise concerns about the sustainability and long-term health effects of such diets, particularly on heart health. For example, ketogenic diets raise LDL cholesterol, which some people believe is harmful.
It’s clear that the question isn’t simply whether carbohydrates or sugars are inherently bad for health, but rather, it’s how they are consumed, in what forms, and in what quantities. In the context of a physically active lifestyle, a higher intake of carbohydrates and even free sugars may not be especially detrimental. It’s also important to acknowledge that each of us respond to nutrients and food differently. Some thrive on a high-carbohydrate diet while others flourish when in ketosis.
So rather than investigate how specific nutrients affect health biomarkers, there’s a growing interest in how restricting or supplying these nutrients might affect physical activity and energy expenditure, key factors in overall health. Some evidence suggests that reducing sugar intake or adopting a low-carbohydrate diet, such as a ketogenic diet, could lead to decreased physical activity energy expenditure. This is particularly concerning as physical activity is not only essential for maintaining energy balance but also plays a critical role in cardiometabolic health, influencing everything from insulin sensitivity to our cardiorespiratory fitness and vascular health.
If restricting sugars or carbohydrates leads to reduced physical activity energy expenditure, it could potentially counteract some of the benefits of these diets, especially in terms of long-term weight management and metabolic health. Being interested in high performance, I might also extend this to athletes. If a particular diet isn’t allowing you to train at your best and adapt to training, is it really good for you?
Understanding how dietary changes impact physical activity energy expenditure and physical activity levels is crucial because it could reveal whether such diets are truly effective or if they carry “hidden risks” for overall health.
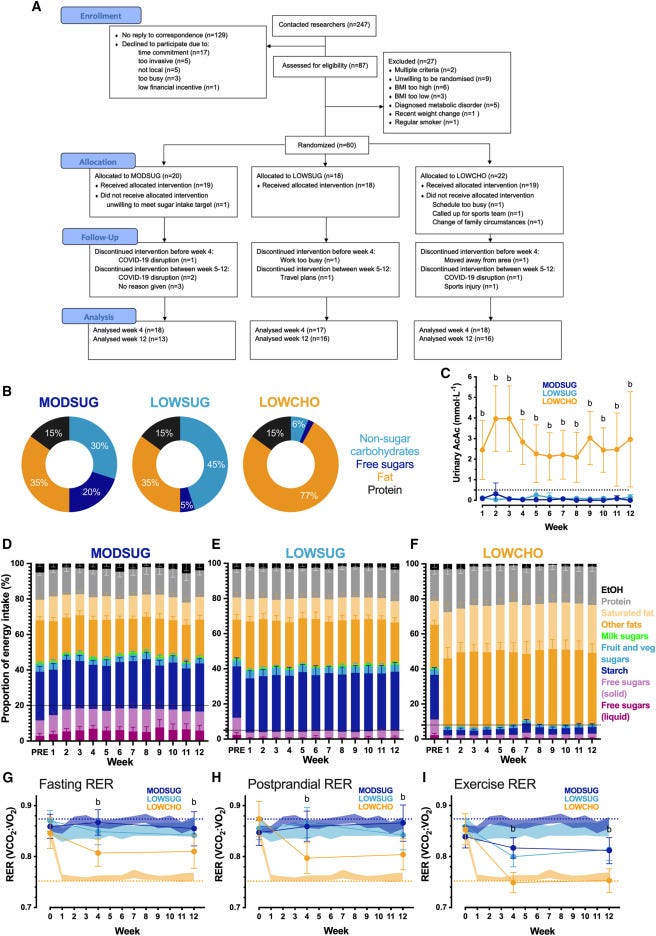
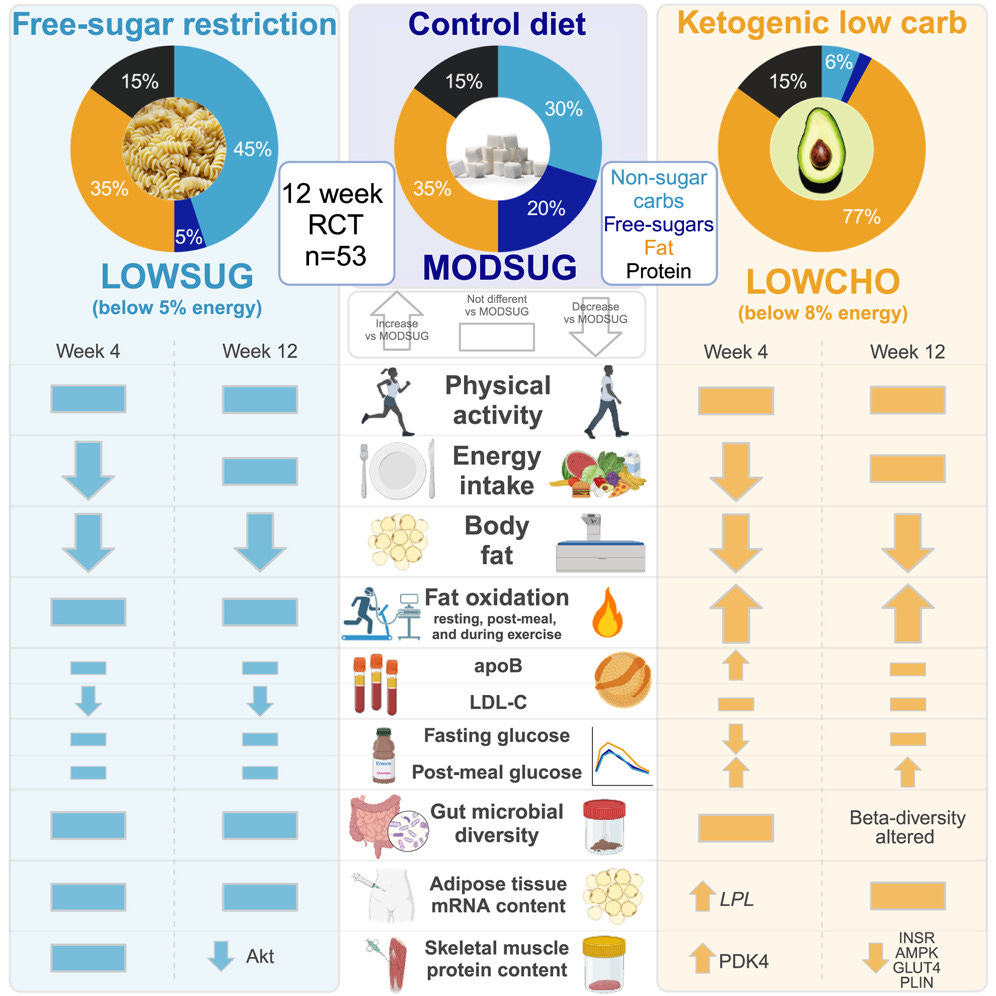
This was the focus of a new study published in Cell Reports Medicine, in which 45 adults (average age of 35; 25 women and 20 men) were randomly assigned to one of three diets for 12 weeks: a low-sugar diet, a low-carbohydrate (i.e., ketogenic) diet, and a moderate-sugar control diet.1
Low-sugar diet: The participants in the low-sugar diet group reduced their free sugar intake to 5% or less of their total energy intake. They accomplished this by limiting their intake of foods with added sugar or naturally occurring sugar found in honey, syrups, and fruit juice.
Low-carbohydrate diet: The participants in the low-carbohydrate diet group restricted their total carbohydrate intake to less than 8% of their total energy intake which was designed to promote a sustained level of ketosis.
Moderate-sugar diet: The participants in this group consumed a diet that was reflective of the macronutrient and sugar intake in high-income countries (actual sugar intake was ~18% of total energy intake throughout the study).
Importantly, the diet interventions were free-living interventions — the participants went about their daily lives and were merely given instructions on what (and what not) to eat.
The efficacy of the diets was assessed by measuring several outcomes before and after the study, which included physical activity levels, metabolism at rest and during exercise, blood glucose control and insulin sensitivity, appetite-related hormones, energy intake, skeletal muscle and fat tissue characteristics, and gut microbiome composition.
Results
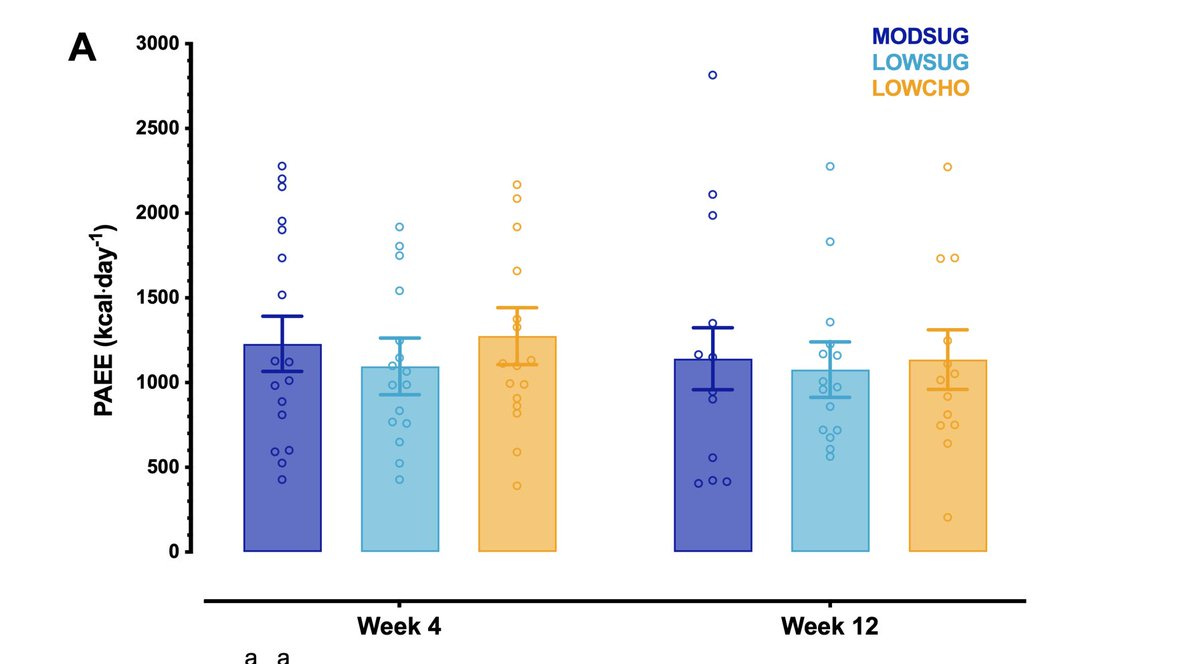
Neither carbohydrate restriction nor sugar restriction reduced the participants’ physical activity energy expenditure compared to the control group. Step counted also remained similar in all of the groups during the intervention.
The participants in the low-carbohydrate diet group experienced an elevation in ketone levels throughout the intervention, and this was accompanied by an elevation in fat metabolism at rest, after eating, and during exercise (indicated by a lower respiratory exchange ratio or RER). No surprises here.
Resting metabolic rate, overnight heart rate, and overnight systolic and diastolic blood pressure were unaltered by carbohydrate or sugar restriction. However, both interventions reduced body mass, nearly all of which was fat mass (about a half a kilogram of 1 pound); in other words, body composition improved.
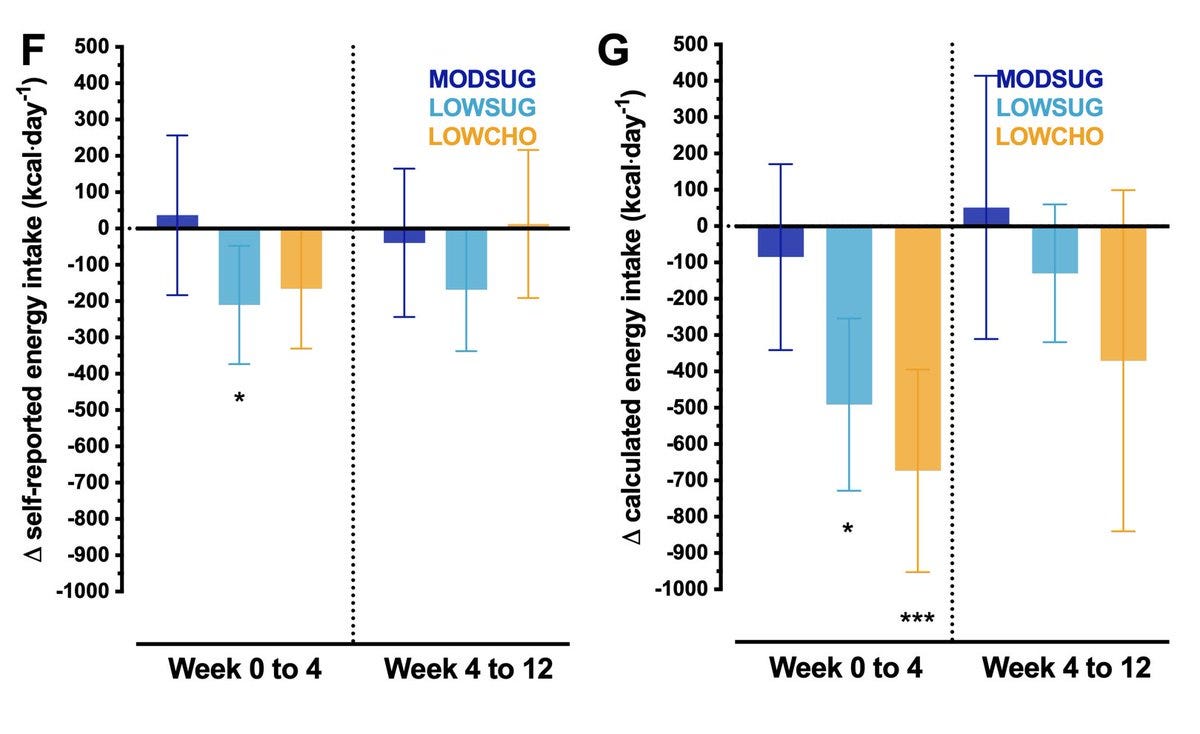
The participants in the sugar restriction group reduced their energy intake by 236 calories per day while those in the low-carbohydrate diet group reduced their energy intake by 172 calories per day compared to baseline. Objectively calculated energy intake decreased by 352 calories per day in the sugar restriction group and by 398 calories per day in the low carbohydrate group.
There were some notable and interesting differences in the diets’ effects on glucose tolerance. The low-carbohydrate diet reduced fasting glucose at week 4 compared to the control group, but by week 12, this difference was no longer apparent. However, the low-carbohydrate diet also reduced (i.e., worsened) glucose tolerance in response to a meal at 4 and 12 weeks — the participants had a higher postprandial glucose response. Sugar restriction didn’t improve fasting glucose but also had no effects on postprandial glucose levels.
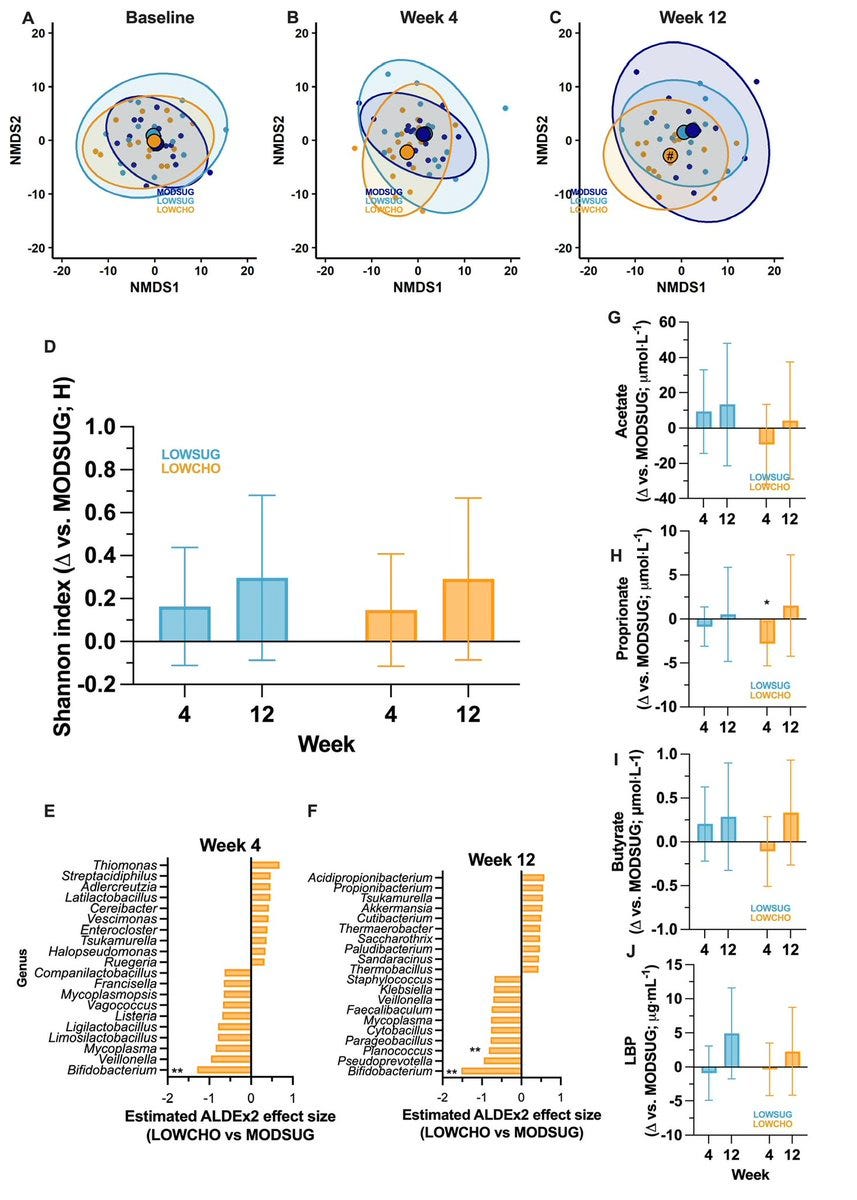
Gut microbiota changes were also observed, with the low-carbohydrate diet causing changes in beta-diversity and reducing the abundance of Bifidobacterium and Planococcus. Other than these changes, no effects of sugar or carbohydrate restriction were observed for microbial alpha diversity or other microbial species.
There were a few changes in skeletal muscle metabolic characteristics that I think are worth noting. With carbohydrate restriction, the skeletal muscle expression of the proteins AMPK, GLUT4 (glucose transporter 4), and INSR (insulin receptor) were reduced — this explains the lowered insulin sensitivity observed after 12 weeks of this diet. AMPK is a protein that’s heavily involved in maintaining energy homeostasis; GLUT4 is important for glucose transport, and INSR is important for regulating the body’s insulin sensitivity. In my opinion, the reduced expression of these isn’t necessarily a good thing from an energy metabolism point of view.
Muscle glycogen levels increased in the sugar restriction group but were unchanged in the low-carbohydrate diet group after 12 weeks.
Lastly, let’s talk about hormones and appetite. Sugar restriction reduced levels of leptin (the satiety hormone) but had no effects on glucagon-like peptide 1 (GLP-1, which you might be familiar with due to the popularity of Ozempic and other GLP-1 agonists), fibroblast growth factor 21, ghrelin (the hunger hormone), or the inflammatory marker C-reactive protein. Carbohydrate restriction reduced leptin and fibroblast growth factor 21 and increased glucagon-like peptide 1.
The diets also had no effect on the participants’ desire for high-carbohydrate sweet or savory foods.
This was a very data- and results-heavy study, so I’m going to do my best to extract some of the key conclusions for you.
Overall, the results show that despite both sugar restriction and carbohydrate restriction (a ketogenic diet) reducing free-living energy intake and reducing body mass, these diets have divergent effects on metabolism and cardiometabolic biomarkers without affecting physical activity.
Restricting sugar or carbs reduces fat mass by around half a kilogram or about 1 pound across 12 weeks. There’s nothing unique about a ketogenic diet or eating less sugar when it comes to fat loss, at least as far as this study is concerned.
This finding actually detracts somewhat from the carbohydrate insulin model of obesity, which posits that weight gain (and loss) are regulated largely by the body’s insulin levels (insulin promotes fat storage). By reducing carbohydrates, we lower insulin levels and therefore, reduce body fat (even in the absence of a calorie deficit). In other words, it’s carbohydrates and not calories that matter.
Yet in this study, the groups lost a similar amount of weight despite one group reducing carbohydrates and the other simply reducing energy intake through sugar (which is, admittedly, a carbohydrate). In fact, starch intake was 160 grams per day in the low sugar group during the intervention and only 15 grams per day in the low-carbohydrate group. A drastic difference in carbohydrate intake that did not manifest in greater weight or fat loss.
Weight loss is all about calories. Who knew.
However, carbohydrate restriction does seem to affect metabolism in a unique way compared to sugar restriction — in ways that can be seen as both positive and negative. Fat metabolism improves, but glucose tolerance (or insulin sensitivity) gets worse and microbiome diversity appears to undergo a few unfavorable changes (Bifidobacterium, which were lower after carbohydrate restriction, are generally seen as health-promoting).
Contrary to what some diet enthusiasts might claim, cutting out carbs and sugar didn’t appear to alter food preferences or food cravings — so much for the idea that eating less sugar means you crave less sugar.
Let’s bring the discussion back to physical activity energy expenditure, as this was the primary outcome after all. Even though the participants in each diet group ate less (300–500 calories per day less on average), they didn’t move less or burn less energy through physical activity.
This is an important finding, because this is a negative “side effect” of some dietary strategies — especially diets that reduce sugar/carbohydrate intake (they’re our energy source after all!)
‘Because physical activity energy expenditure didn’t change, the weight loss achieved by the participants was entirely explained by changes in energy intake rather than energy output.
What can we learn from this study? Well for one, it’s impossible to conclude that any one diet is “good” or “bad.” As we can see, restricting sugar or restricting carbohydrates had beneficial, neutral, or adverse effects depending on the outcome being studied. In other words, no single diet will improve every measure of health. If improving fat metabolism is your primary goal then sure, restricting carbohydrates via a ketogenic diet is probably the best approach. That’s if you don’t care about higher cholesterol levels and other potentially negative cardiometabolic outcomes that might be associated with this dietary approach.
But if you simply want to lose weight and aren’t willing to risk higher cholesterol or a potential reduction in your glucose tolerance, then maybe it’s best to just eat less sugar.
This wasn’t meant to be the definitive diet study to crown the champion way of eating. Rather, I think it’s a beautiful (and dense) illustration that the interaction between food and our physiology is complex, and only by rigorously experimenting (in the lab or more importantly, on ourselves) can we learn which way of eating works best for us.
That’s a sweet conclusion.
Thanks for reading. See you next Friday.
~Brady~
The VO2 Max Essentials eBook is your comprehensive guide to aerobic fitness, how to improve it, and its importance for health, performance, and longevity. Get your copy today and use code SUBSTACK20 at checkout for a 20% discount. You can also grab the Kindle eBook, paperback, or hardcover version on Amazon.
Examine.com: Examine is the largest database of nutrition and supplement information on the internet.




That is a super interesting (and very well explained) break-down of this study. Due to some microbiom dysbiosis, i have been following a ketogenic diet for quite a while now.
It is interesting to see that increase in insulin/glucose sensitivity with the low-carbohydrate group. I am wondering if it is really a negative effect since isn't that what our natural metabolisms are designed to? To have like super high energy available if we eat a high-glucose food just on it's own? (Like which other omnivore out in the wild does that even?).
I am a bit concerned about the long-term effects related to the good bacteria (which I just try to re-cultivate 🤣). So it might be that the ketogenic diet can have overall health benefits but not as a long-term lifestyle (but more like cycling it into a more natural rhythm), but including some natural sources of sugar and starch again at times to keep the microbiom happy.
This is a fascinating article; well done.
As I am keto-flexing right now (5 days intermittent fasted keto, 2 days more normal diet), I can attest to the fact that low-carb does reduce sugar cravings for me, on about day 2 of keto.
There are major differences between the approaches of keto or just cutting sugar for endurance activity, like long-distance sports, bricklaying, and other hard physical jobs.
I'm a runner. I can have zero carbs for several days and then run for an hour with energy left to spare. I never seem to run out of energy,even if I've fasted for 24 hours. So this is one advantage I get from ketogenic diet that I would NOT get from simply cutting sugar. When I have only cut sugar, I have to eat way more frequently.