Physiology Friday #234: Is It Time to Retire the Idea of the "Healthy Sedentary" Person?
Compared to active adults, inactive ones display metabolic, mitochondrial, and cellular dysfunction at rest and during exercise.
Greetings!
Welcome to the Physiology Friday newsletter.
Thanks to the premium sponsor of this newsletter: FSTFUEL electrolyte supplement.
FSTFUEL combines electrolytes with amino acids to help your body maintain hydration and optimal functioning during exercise or intermittent fasting, so you don't have to choose between fasting and fitness. It’s a zero-sugar electrolyte drink that tastes awesome. I use it every single day (no really, I do).
If you want to try some, the guys at FSTFUEL have agreed to give my audience a 30% discount on their orders. Just use the coupon code BRADY30 at checkout.
Details about the other sponsors of this newsletter including Examine.com and my book “VO2 Max Essentials” can be found at the end of the post!
Sedentary (adj.): Of occupations, etc., "requiring much sitting," by c. 1600. In reference to persons, "accustomed to long sitting," 1660s, hence "inactive, not in the habit of exercise." Related: Sedentariness.
Diabetes, cardiovascular disease, cancer, Alzheimer’s disease, depression.
What do all of these things have in common?
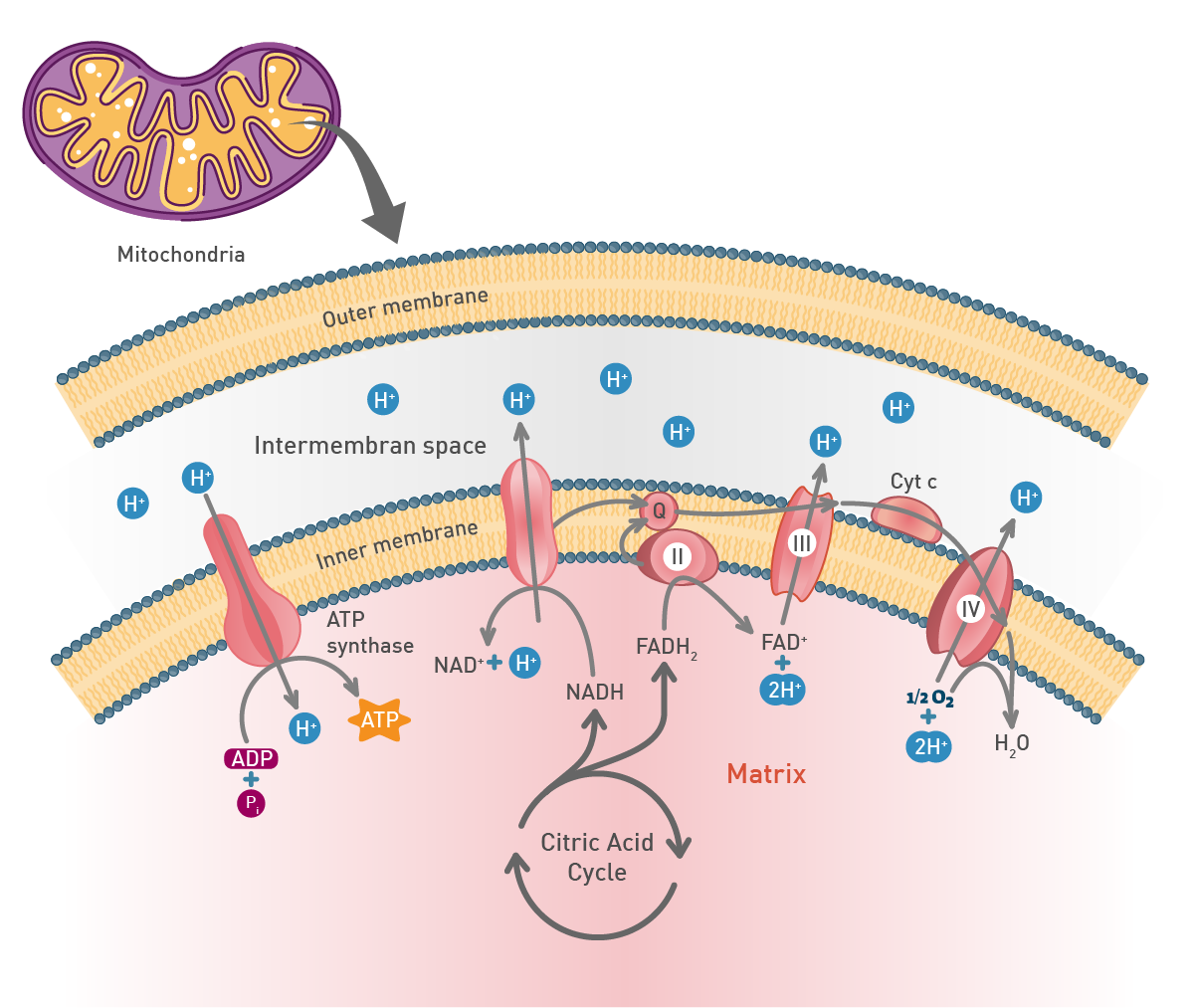
Not only are they the leading causes of (preventable) death around the world, but they also share one underlying pathology: mitochondrial dysfunction.
What’s the main cause of mitochondrial dysfunction? Inadequate physical activity.
I’m not saying that if everyone just exercised more, then we’d obliterate diseases of modernity overnight (but maybe?)
However, there is no doubt that if, as a population, we exercised a bit more, rates of these and other diseases would drop precipitously. If you need evidence, consider that only one-fourth of adults meet the minimum recommended physical activity levels each week. We’ve got some major work to do.
As an intervention, physical activity changes lives, reduces healthcare expenditures, and increases human flourishing. As a self-proclaimed “exercist”, I don’t think there’s a malady that doesn’t improve when someone starts exercising more.
But maybe the problem is that we’re thinking about physical activity all wrong.
For decades, researchers have argued that because humans evolved to be physically active, people who exercise are actually “normal” in an evolutionary context, whereas inactive individuals should be seen as outliers. Sedentariness is a dangerous experiment that many people participate in each day.
We normalize inactivity and see physical activity as a deviation from the norm. But it should be the opposite.
Anyone familiar with clinical research is well aware of this. Control groups of subjects in an experiment typically comprise individuals who are not regular exercisers but who also don’t have any known diseases — a so-called “healthy sedentary” control group. These control groups are often used to determine the effects of an exercise intervention or to compare and contrast different groups of people (say older people or elite athletes) in a cross-sectional study.
But how healthy can one be if they’re also sedentary? Does a lack of disease imply the presence of good health? Perhaps metabolic function earlier in life can be used to detect the onset of disease long before “modern medicine” actually gives a diagnosis.
These are all questions that haven’t been adequately addressed by science but have the potential to influence the research process, public health policy, and perhaps your own actions.
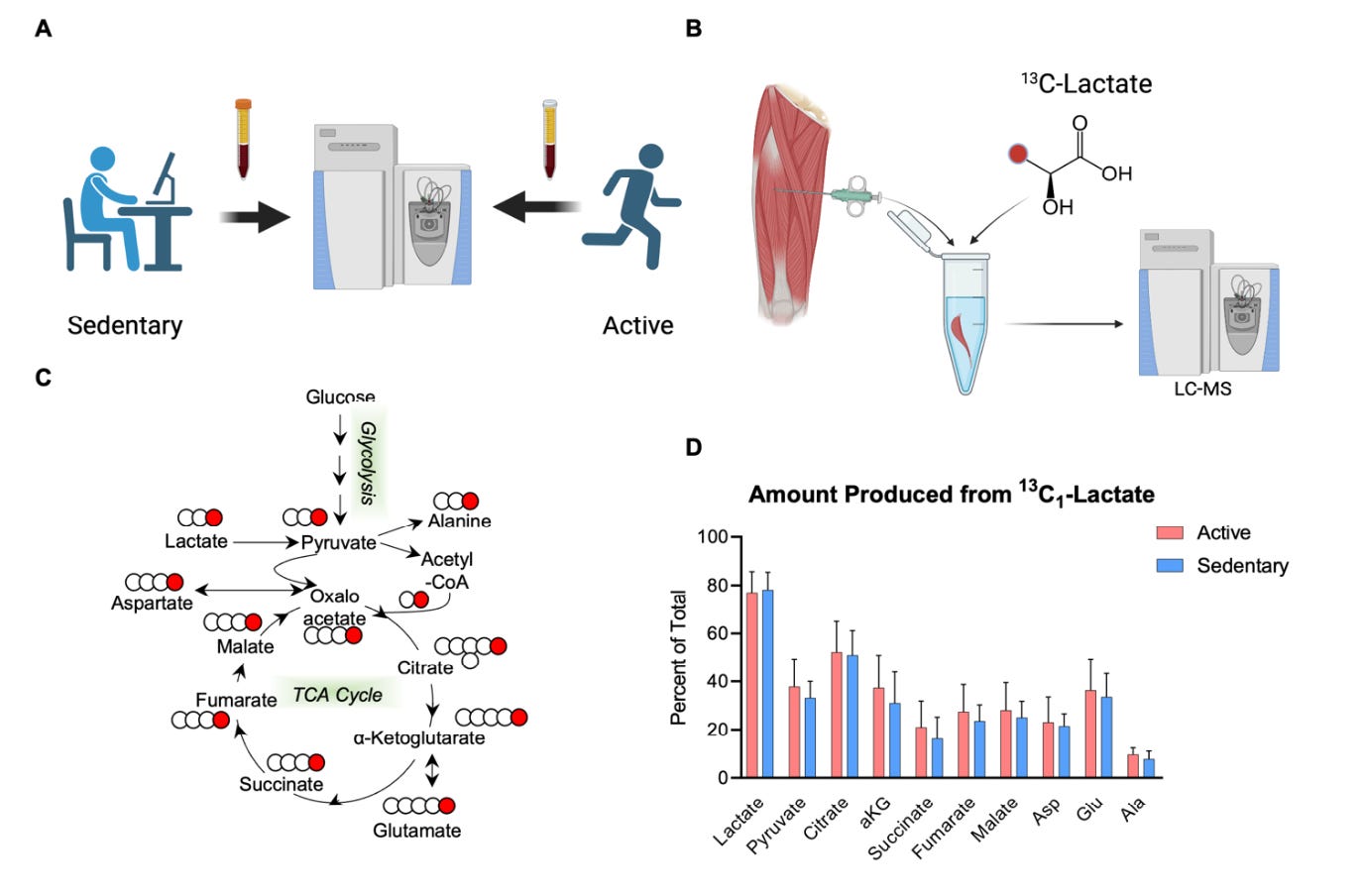
A new study (published as a pre-print) from Dr. Iñigo San Millán and colleagues set out to investigate the metabolic, cellular, and mitochondrial differences between inactive but “healthy” adults and a moderately active group — what they refer to as the “evolutionary control cohort.”1
For the study, a total of 19 men with an average age of 42 were characterized into one of two groups:
A sedentary group (10 participants): These men did not perform regular exercise.
An active group (9 participants): These men performed aerobic exercise for at least 150 minutes per week for a minimum of 6 months.
The participants were characterized at rest using multiple assessments of skeletal muscle and mitochondrial quality. They were also characterized during exercise using a maximal exercise test to exhaustion, during which carbohydrate and fat oxidation rates and lactate clearance were assessed to determine mitochondrial function and metabolic flexibility. For the exercise test, all of the participants cycled at 75 Watts to start, after which the intensity increased by 10 Watts per minute until they voluntarily stopped pedaling due to exhaustion — a point representing their maximal oxygen consumption or VO2 max.
At rest, the active group demonstrated superior mitochondrial function as indicated by higher activity of mitochondrial complexes I and II, a greater capacity of the electron transport chain to produce energy (ATP), and a better ability to oxidize fat, pyruvate (a product of carbohydrate or glucose breakdown), and amino acids. In other words, active people are better energy producers at rest. Though not statistically significant for most measures, the sedentary group produced more reactive oxygen species per unit of oxygen consumed compared to the active group.
While the active and sedentary groups had a similar number of glucose transporters and lactate-metabolizing enzyme protein expression in their muscles, the active group had higher levels of mitochondrial pyruvate carrier 1 (MPC1) and the mitochondrial fatty acid transporter carnitine palmitoyl transferase 1 (CPT1). These are proteins that transport pyruvate and fatty acids into the mitochondria — explaining the lower ability of this group to use pyruvate and fatty acids for ATP production.
Now let’s move on to the exercise assessments.
The first finding is that — unsurprisingly — the sedentary participants had a lower cardiorespiratory fitness (VO2 max) than the active participants. While the data were only provided in the form of a graph (see below), it appears that the VO2 max of the sedentary group was somewhere around 25–30 ml/kg/min, while that of the active group was around 45–50 ml/kg/min: this corresponds to a 38% higher VO2 max in the active group.
The active participants also had a 42% higher maximal power output (~225–250 Watts) than the sedentary participants (~150 Watts) and a superior lactate clearance capacity at a power output of 125 and 150 Watts.
Put another way, blood lactate was higher at 125 Watts (~4.5 mmol) and 150 Watts (~6 mmol) in the sedentary group than in the active group, for whom lactate levels reached ~1 and ~2 mmol at 125 and 150 Watts, respectively.
When the active participants were exercising in zone 2, the sedentary participants were well above what we’d consider their lactate threshold!
Things get incredibly interesting when we look at substrate oxidation during exercise.
Let’s first look at the results for the active participants (panels A, C, and E in the graph below). As exercise starts, their lactate levels are low and their fat oxidation rates are high (panel A). As exercise intensity increases, lactate levels naturally rise and fat oxidation levels naturally fall, but fat oxidation never reaches zero, even at the participants’ peak power output at the end of the test (when they reached VO2 max).
In panel C, we can observe the expected rise in carbohydrate oxidation and the fall in fat oxidation during the graded exercise test, and see that the average “crossover point” (when carbohydrate and fat oxidation meet) occurs right around 175 Watts — 70% of their maximal intensity; this is when carbohydrates become the dominant fuel source.
Now let’s take a look at the sedentary group, who already began the exercise test with higher blood lactate levels and almost half the rate of fat oxidation compared to the active participants (panel B below).
Unlike the active participants, the sedentary participants eventually bottom out their fat oxidation rates at a power output of around 175 Watts. Even more interesting is the fact that the “crossover point” for carbohydrate and fat oxidation in the sedentary participants happens almost immediately after the test begins — less than 100 Watts!
Carbohydrates become the predominant fuel source at an intensity corresponding to 30% of their maximal power output. This indicates a profound lack of metabolic flexibility.
The higher rates of fat oxidation in the active people and lower rates of fat oxidation in the sedentary people were strongly correlated with their mitochondrial function measures discussed above. The better the mitochondrial function, the better the ability to use fat as a fuel during exercise.
I want to underscore a finding that was highlighted by the authors — and that is the lower capacity of the sedentary group to transport and metabolize pyruvate. Pyruvate is what’s left over after a molecule of glucose or glycogen is broken down during glycolysis — the process our body uses to eventually create energy (ATP) from carbohydrates (really, glucose). Pyruvate is then transported into mitochondria where it’s used to produce energy, while some is converted into lactate.
What’s interesting is that the sedentary participants did not have fewer glucose transporters in their muscles when compared to the active group. Glucose transporters — specifically GLUT4 — are critically important for insulin- and exercise-mediated increases in glucose uptake into muscle cells. Insulin resistance (characteristic of type 2 diabetes) causes a dysregulation in GLUT4 translocation and glucose uptake capacity.
Dysregulated pyruvate metabolism could be the initial cellular indicator of metabolic dysfunction, something that occurs before insulin resistance and elevated blood glucose levels. Mitochondrial dysfunction may be the canary in the coal mine for later metabolic disease.
The sedentary participants may not have diabetes now, but they might later.
What’s also important (and clinically relevant) is the fact that several indicators of early metabolic dysfunction were identified during a simple treadmill test — something anyone could perform at a clinic or university research laboratory. Two measures — oxygen uptake and blood lactate — could provide unprecedented insight into how the body works and identify people at risk for conditions that might not present for several years to decades. Treadmill testing could be the microscope into the undiscovered world of metabolism.
These findings have profound implications for how we classify and recruit participants in research studies. They suggest that the “healthy sedentary” phenotype doesn’t exist — a lack of disease does not imply someone is in good metabolic health. As such, we shouldn’t be using these “healthy sedentary” people as control subjects in studies.
Instead, moderately active people who meet the physical activity guidelines should be used as the proper control group because they represent normal metabolic function, the standard by which we should judge our interventions.
Finally, remember that these weren’t high-level athletes in the active group, just guys who exercised about 3 times per week for an hour at a time, and they still had superior function across nearly all measures of metabolic and mitochondrial function at rest and during exercise. That’s a friendly reminder that it doesn’t take much to be above average in modern-day society — just get moving! Your mitochondria will thank you.
Thanks for reading. See you next Friday.
~Brady~
The VO2 Max Essentials eBook is your comprehensive guide to aerobic fitness, how to improve it, and its importance for health, performance, and longevity. Get your copy today and use code SUBSTACK20 at checkout for a 20% discount. You can also grab the Kindle eBook, paperback, or hardcover version on Amazon.
Examine.com: Examine is the largest database of nutrition and supplement information on the internet.
FSTFUEL combines electrolytes with amino acids to help your body maintain hydration and optimal functioning during exercise or intermittent fasting, so you don't have to choose between fasting and fitness. If you want to try some, the guys at FSTFUEL have agreed to give my audience a 30% discount on their orders. Just use the coupon code BRADY30 at checkout.








Fantastic! More proof that exercise is the ultimate medicine.
For the record, I always thought that sedentary meant “unhealthy,” because how could it not?
And. If you aren’t exercising and fit, you’d last minutes during an emergency, let alone a zombie apocalypse.
Thank you for a great article! If pyruvate could be an early diagnosis for risk of insulin resistance and type 2 diabetes then what level could it be an indication for that risk? And could type 2 diabetes be reversed with exercise only?