Physiology Friday #276: Heat, But Not Cold, Promotes Muscle Regeneration After Injury
One more reason why "put some ice on it" is terrible advice.
Greetings!
Welcome to the Physiology Friday newsletter.
If you’ve jumped on the creatine bandwagon (who hasn’t) but aren’t sure where to start, I suggest you try out Create—the first “modern creatine” brand. They sell a wide range of gummies (including a new sour cherry flavor), flavored creatine monohydrate single-serve packets, and even a daily performance mushroom & greens gummy (my personal favorite).
They’re giving my audience 25% off of their entire order. So stock up!
Details about the other sponsors of this newsletter, including Ketone-IQ, Examine.com, and my book “VO2 Max Essentials,” can be found at the end of the post. You can find more products I’m affiliated with on my website.
Rest, Ice, Compression, Elevation.
That used to be the standard advice in the sports medicine world after you got injured. Problem is, it was all wrong—at least the “Ice” part.
Dr. Gabe Mirkin coined the acronym in 1978, cementing (perhaps freezing is a better word ice as a standard treatment for injuries and sore muscles. The cold (so it was thought), helped relieve pain caused by injured, inflamed tissue. Stop the activity (Rest) and numb the area (Ice) was seen as the most effective way to kick-start recovery and regeneration.
But as science has advanced, we’ve learned that both ice and complete rest might actually delay healing instead of help it. The RICE protocol completely ignored the need for early loading and inflammation-driven repair. Inflammation is not the enemy when it comes to healing and adaptation. The first 24–72 hours are dominated by pro-inflammatory macrophages that clear debris and release insulin-like growth factor 1 (IGF-1)—signals that summon satellite cells and start rebuilding muscle fibers. Suppressing that response slows everything that follows. That applies whether your goal is to heal an injury or build bigger muscles.
What actually happens when you ice an injury (or use whole-body cryotherapy/cold water immersion)? Rapid cooling constricts blood vessels, cuts muscle blood flow, and even slows nerve conduction velocity. That’s what gives the short-lived analgesic (pain-reducing) effects. But the same mechanism that helps with pain hurts healing. Pro-inflammatory cells don’t infiltrate the injured area as effectively and the delivery of oxygen and nutrients is reduced drastically.
Hence why repeated post-work-out cold-water immersion blunts anabolic signalling, protein synthesis and hypertrophy gains.
Recent recommendations are thus to use ice sparingly (≤10 min, separated by re-warming, only in the first hours) if pain is the priority, but don’t expect it to heal the tissue. Even Dr. Mirkin publicly retracted blanket icing in 2015, noting it can “delay healing instead of helping.”
Instead, the focus has now shifted to heat.
In contrast to cold, heat opens blood vessels, increases oxygen delivery, and jump-starts muscle repair machinery. It up-regulates heat-shock proteins, speeds the shift from pro- to anti-inflammatory macrophages, and boosts satellite-cell proliferation. This accelerates fiber maturation and even appears as effective as cold for reducing pain and muscle soreness. And the biology makes perfect sense.
When muscle is torn or strained the first 48 h are dominated by pro-inflammatory macrophages that clear debris. Moving into the growth phase requires a switch to perfused, warm, anti-inflammatory tissue, entry of satellite (stem) cells, and activation of the protein-synthesis machinery. Raising intramuscular temperature by just a few degrees with a sauna session, hot-water immersion, or a hot heat pack accelerates nearly every one of those steps.
Even though heat and cold have been investigated separately for their ability (or lack thereof) to heal muscle injuries, few studies have compared them using a practical experimental model in humans. A new study did just that, and the results will shift the way you tackle recovering from your next injury.1
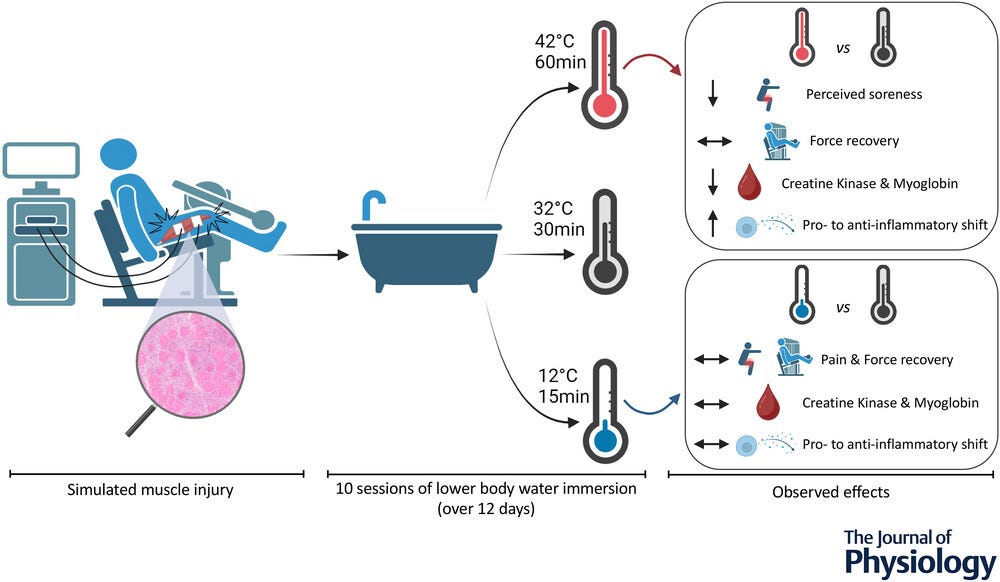
Researchers put 34 former athletes and current “fitness enthusiasts” (all men) through a muscle-damaging protocol designed to induce significant myofiber necrosis (cell death) in the quadriceps muscle, conditions favorable for studying the regeneration process in detail.
This wasn’t your average “workout to get sore.” Electrical stimulation was administered through electrodes placed strategically on the quadriceps muscle. A total of 200 electrically stimulated eccentric contractions, split evenly between a slow and fast velocity, were performed for each participant (eccentric or lengthening contractions are those that lead to more muscle damage…they’re why you feel sore after certain types of exercise). This protocol successfully induced muscle injury, evidenced by signs of myofiber necrosis and significant declines in muscle strength: The participants' ability to generate force decreased by 59% 2 days after the protocol and remained 32% lower 10 days after. That’s some major damage.
One of three different thermal “recovery” protocols was implemented beginning one hour post-injury and repeated daily for 10 days after. All of them involved sitting waist-deep in a temperature controlled bath.
Here’s what each looked like:
Cold water immersion: 12°C (53℉) for 15 minutes
Hot water immersion: 60 minutes at 42°C (107℉) for 60 minutes
Thermoneutral water immersion (the control condition): 32°C (90℉) for 30 minutes
Across the board, heat was not only the more effective, but the only effective treatment.
Participants in the hot water immersion group experienced less quadriceps muscle pain (when they applied pressure to their thigh, but not during a bodyweight squat), and even though their muscle strength (measured as their maximal force production) didn’t fully recover, even 10 days after the injury, they had a smaller decline in force production 4 days after the injury (a 31% reduction compared to baseline) compared to the other groups, whose force production was nearly 50% lower at the same time point. So, while not completely regenerative, heat appeared to mitigate the drop in muscle performance after an injury. With less soreness too.
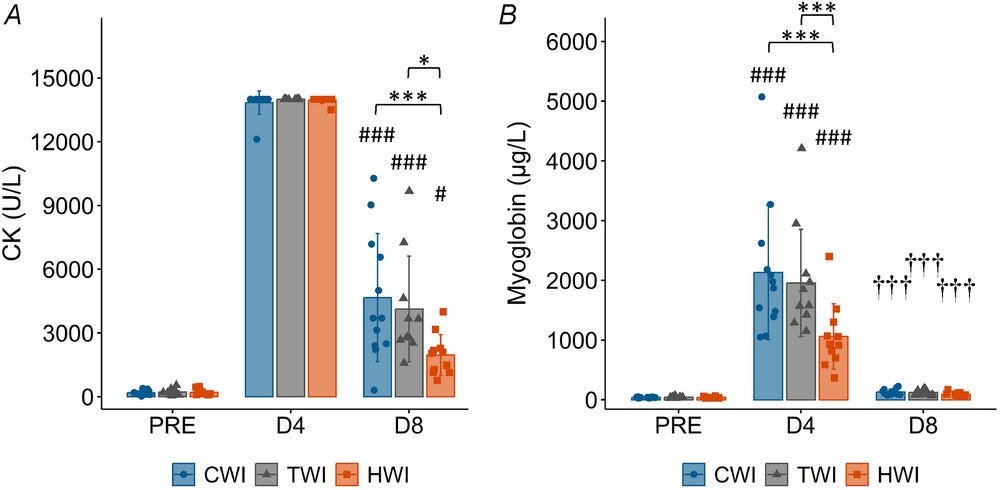
Heat also shined for reducing markers of muscle damage—with notably reduced creatine kinase and myoglobin levels compared to the cold and thermoneutral water conditions. That’s likely due to enhanced blood flow allowing greater clearance of these injury-related metabolites. A more favorable inflammatory profile was also observed with hot water immersion, with stable levels of p-NF-κB and increases in IL-10. The expression of heat shock proteins 27 and 70 (HSP27 and HSP70, respectively) increased throughout recovery in the hot water immersion group, which is a likely mechanism governing quicker recovery since these so-called stress response proteins contribute to cellular protection and other adaptive mechanisms.
In short: accompanying the changes in physical and perceptual muscle recovery was an earlier shift from a pro-inflammatory to an anti-inflammatory stage of the recovery process.
Now for the surprising part(?) None of these benefits were observed in the cold water immersion group—there was no improvement in pain, muscle soreness, or markers of muscle damage compared to the other treatments; a blunted heat shock protein response; and an unfavorable inflammatory response characterized by increased p-NF-κB expression and unchanged IL-10 levels.
One thing worth noting. Despite differences in molecular markers and pain, which overall favored the hot water immersion group, no significant differences were observed for muscle strength recovery across treatments (despite those small differences at some time points discussed earlier). None of the groups fully recovered their maximal strength by the end of the study (day 10), observable in the graph below.

This post has already been somewhat verbose, so I won’t reiterate anything I’ve said and will jump to the conclusion.
What we have here is yet another study showing that there doesn’t seem to be much that cold is good for, and that includes the main mechanism by which it’s proposed to promote recovery—reducing muscle pain and soreness. And here’s an even more powerful nugget from the study. The researchers “noticed a strong positive belief towards the efficacy of [cold water immersion] among participants.”
Even though the participants thought that the cold would provide a more regenerative and pain-reducing stimulus, it didn’t. Sometimes, actual physiology is no match for the placebo effect.
Writing about research on heat seems to be a theme for me lately (it’s summer after all), but that’s because there’s so much interesting data on its power to heal, promote health, and even enhance performance when added to endurance or resistance exercise training. It’s a powerful stimulus that really taps into our biology to produce meaningful effects.
If you’re injured (or planning on it), keep hot water immersion in your toolkit. Start it early after injury and keep it up throughout the recovery process.
If you’re not injured, the heat can be just as powerful for promoting recovery from a demanding workout. Use liberally.
Thanks for reading. See you next Friday.
~Brady~
The VO2 Max Essentials eBook is your comprehensive guide to aerobic fitness, how to improve it, and its importance for health, performance, and longevity. Get your copy today and use code SUBSTACK20 at checkout for a 20% discount. You can also grab the Kindle eBook, paperback, or hardcover version on Amazon.
Examine.com: Examine is the largest database of nutrition and supplement information on the internet.
Ketone-IQ is high-performance energy in a bottle. I use it for post-exercise recovery along with enhancing focus, mood, and cognition. Take 30% off of your order.







This is a neat finding. I often recommend heat over ice in the clinic. And now there’s some science behind it.
Any thoughts on foam rolling, massage, Thera Gun type stimulus or the like combined with/during a sauna. Once the deeper muscle temperature increases (15-20 minutes) might beneficial effects of massage be amplified?