Sleep and Cardiovascular Disease Part II: Circadian Rhythms & Heart Health
The role of biological clocks in sleep, and how their disruption leads to disease.
Greetings!
Last week, I released part I of an ongoing blog series on sleep and cardiovascular health.
This week, in part II, we will talk about how circadian rhythms govern our sleep and biological processes — and how a disruption of these biological clocks can lead to diseases of the cardiovascular system.
Here’s what to look forward to in the remaining parts of this series:
Part III: Sleep Deprivation and Blood Vessel Health
Part IV: Mechanisms Underlying the Effects of Sleep Loss on Cardiovascular Disease Risk
Part V: How Exercise Protects against the Effects of Sleep Loss
In part I of this series, we established that sleep deprivation is associated with adverse cardiovascular outcomes. In addition, we looked at studies showing sex differences in the strength of the association among insufficient sleep duration and CVD. The conclusion, it seems, is that women might suffer more from the effects of short sleep than men, though more evidence is needed.
Exploring associations is worthwhile, but where this topic really gets fun is when we start to explore what might be underlying these associations; that is, by what mechanism(s) does a lack of sleep promote cardiovascular dysfunction.
While we will talk about some specific biochemical and hormonal mechanisms in a future post, one of the most plausible mechanisms linking sleep and CVD involves circadian rhythms.
Circadian rhythms: an overview ⏰
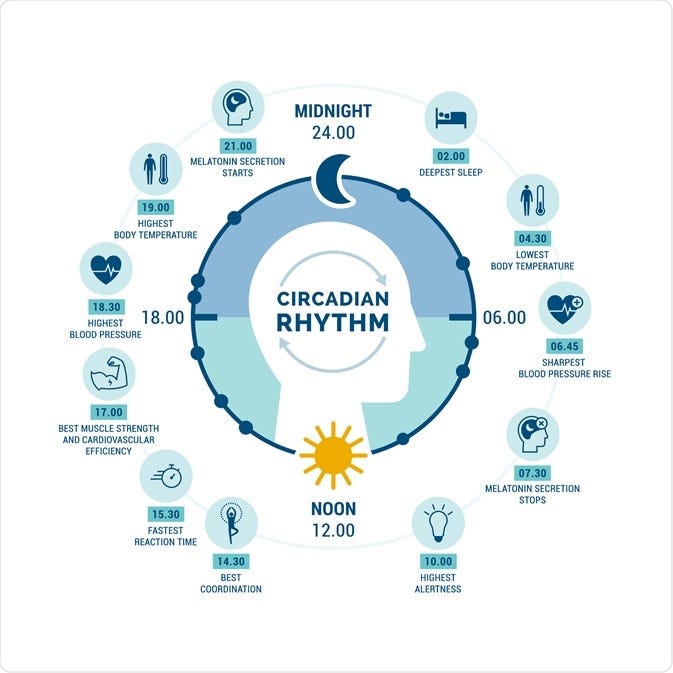
Briefly, circadian rhythms (from circa dia meaning “about one day”) are internal 24 hour clocks present in nearly all of our cells. They control processes like sleep and eating behavior, hormone release, and even some aspects of muscle performance.
An area of the brain known as the suprachiasmatic nucleus (SCN) is known as the “master regulator” of our body’s circadian rhythm, however, all of our organs have their own internal clock.
We have circadian rhythms in our cardiovascular system too.
Throughout any given day, there is a considerable variation in blood pressure, blood clotting, and the ability of our blood vessels to relax (known endothelial function).
One well-known example of cardiovascular circadian rhythms is the fact that our blood pressure drops during the night, or so called blood pressure dipping.
People who are “non-dippers” (their blood pressure fails to drop overnight) are shown to be at an increased cardiovascular disease risk compared to those whose blood pressure dips during the nighttime. Blood pressure dipping seems to have a health-protective function, a lack of which predisposes to disease.
Endothelial function also exhibits a circadian rhythm. Our blood vessels have a greater ability to dilate in the afternoon compared to the morning.1
Not surprisingly, reduced endothelial function in the morning also corresponds to a morning surge in blood pressure. This explains the fascinating observation that there is a higher prevalence of cardiovascular events like heart attack and stroke in the morning.2 This statistic can likely be explained, in part, by circadian rhythms that cause the morning spike in blood pressure and cortisol (and perhaps exacerbated by a.m. rush hour).
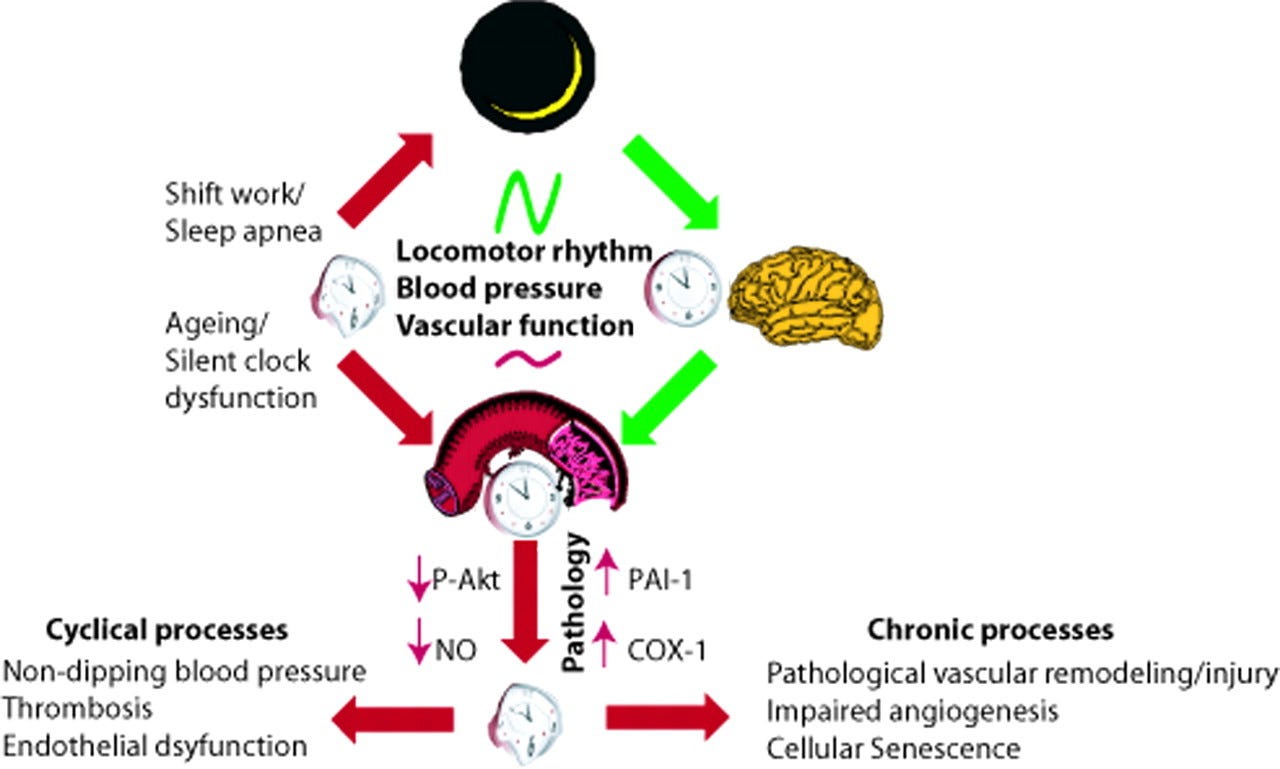
Failure to get enough sleep — or sleeping at the “wrong” time for your body (delaying bedtime or working the night shift, for instance) — can disrupt the normal daily fluctuations in vascular function, blood pressure, and other cardiovascular processes.
If internal clocks lose their synchronicity with the external environment and daily activities, our body becomes unable to properly regulate crucial functions.
There are data to indicate that circadian disruption impairs cardiovascular function. For instance, animals who have had their internal circadian clocks altered, or “knocked out” via experimental manipulation have impaired endothelial function and show evidence of accelerated cardiovascular aging.3
How do sleep deprivation and sleep loss contribute to circadian disruption? 😴
One could theoretically be sleep deprived while still having a “normal” circadian rhythm — maintaining a regular sleep schedule but only getting 4 hours of sleep per night, for instance.
Poor sleep habits and “social jetlag” may better explain circadian misalignment than simply not getting enough sleep.