The Latest Evidence on Atherosclerosis in Athletes
Does "extreme" endurance exercise harm the heart?
If you exercise, you’ll probably live longer than someone who doesn’t.
But can you exercise too much?
Athletes at all levels love to push themselves to the extremes. That’s why marathons, ultramarathons, Ironman triathlons, and other crazy endurance races have become so popular.
Like anything — food, alcohol, work — exercise can also be overdone. Most exposures in life operate on a bell curve, where “too much” and “not enough” are harmful, and somewhere in the middle is “just right”.
It’s well-known that the cardiovascular benefits of exercise begin at a pretty low level — the greatest benefit is achieved when one goes from doing nothing to doing something.
There’s more debate about the optimal level of exercise for reducing the risk of death and disease. In my humble opinion, the current recommendation of 150 minutes per week of moderate-intensity or 75 minutes per week of vigorous-intensity (aerobic) exercise is a bit too low, despite the fact that less than a quarter of people are able to achieve it.
Doubling this amount to 300 minutes of moderate-intensity or 150 minutes of vigorous-intensity activity per week would (if adhered to, of course) yield massive benefits for cardiovascular health. Remember that cardiovascular disease is the leading cause of death around the world. Something’s gotta give.
So — we know that some exercise is good and more is better, to a point.
But in the last decade, a few cross-sectional studies have indicated that high-volume exercise might be risky for heart health. When comparing athletes to control groups (i.e., people from the general population), coronary artery calcium scores (CACS) are higher, indicating more calcification and the presence of atherosclerotic plaques. Among athletes, those who are more active have even higher CACS than those who are less active.
There are a few pieces of evidence, however, that can give endurance athletes some reassurance that they’re not headed to an early grave.
For one, athletes live longer than the general population, with reductions in all-cause and cardiovascular disease mortality of about 30–40%.
A review article on “Mortality and longevity of elite athletes” found something similar: elite endurance (aerobic) athletes and mixed-sports (aerobic and anaerobic) athletes survive longer than the general population as indicated by both lower mortality and higher longevity (lifespan), which was explained primarily by a lower cardiovascular mortality.
Specifically, long-distance runners and cross-country skiers lived 2.8–5.7 years longer than the reference populations (likely also due to their incredibly high VO2 max scores). Athletes in sports like soccer, ice-hockey, basketball, and track and field also survived about 4 years longer than the reference populations.
This at least informs us that high-level athletics does not seem to compromise longevity or increase one’s risk of death. We cannot, of course, infer causation from these observations.
Even among non-athletes, higher levels of activity appear to be beneficial.
There is a consistent dose-response relationship between physical activity volume and CVD and all-cause mortality. The same thing is often observed for weekly or daily step counts, and I don’t think we have enough data to indicate that there’s an upper limit to the benefits of physical activity.
Second, a high VO2 max is one of the most potent predictors of all-cause mortality. Individuals with greater levels of aerobic fitness have lower all-cause mortality compared to less-fit individuals, with the lowest risk observed in people with so-called “elite” levels of aerobic fitness.
Third, even though a greater plaque presence has been observed in some athletic cohorts, the plaque composition may be less harmful, characterized by more calcified and less mixed plaques.
Calcified plaques are known to be more stable and less prone to rupture and lead to a heart attack. In other words, even though athletes may have more plaque, the plaque composition may be more benign and thus, not be associated with a greater cardiovascular disease risk.
A number of cross-sectional studies have supported this hypothesis. Quick note: most of the currently available evidence is in middle-aged and older men, and thus may not apply to younger athletes or women. In fact, there’s not yet any evidence that women who exercise a lot have higher CACS compared to non-athletes.
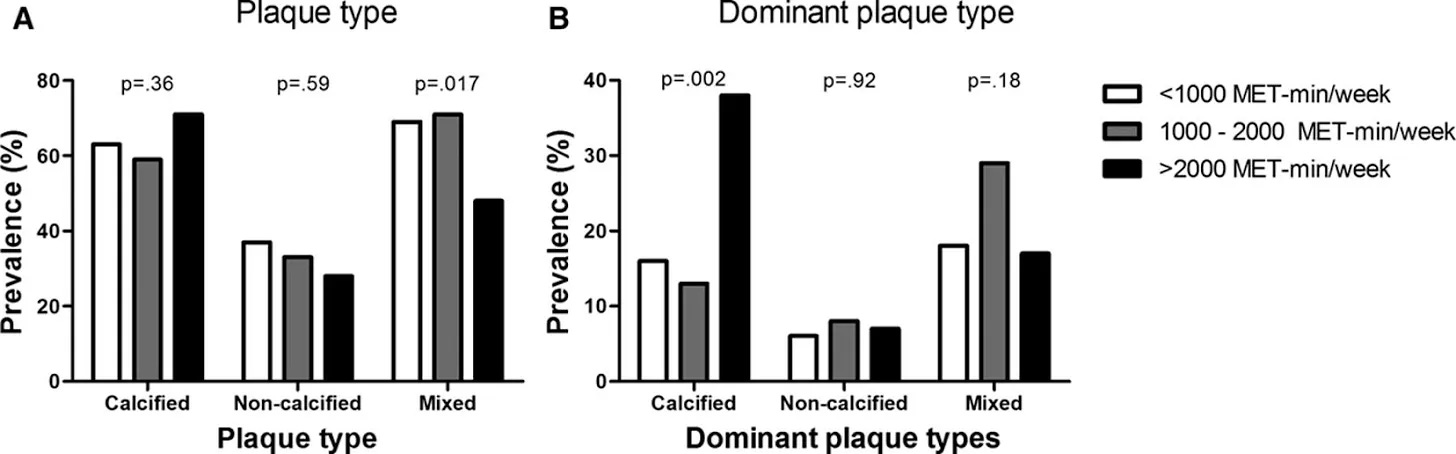
In a study known as the Measuring Athletes’ Risk of Cardiovascular Events or MARC study, the most active participants had more calcified plaques and fewer mixed plaques compared to the least active participants.
Athletes who reported the greatest volume of lifelong exercise — about 6 hours per week of exercise from age 12 onward — were more likely to have a CACS > 0. The most active group also had a greater prevalence of any type of plaque compared to the least-active group (who reported a lifelong exercise volume of around 1.5 hours per week).
Moderate- and vigorous-intensity exercise weren’t associated with the risk of CAC or plaque, but very-vigorous-intensity exercise was. The more time devoted to very-vigorous-intensity exercise each week, the greater the presence of CAC and plaque.
But the types of plaque were different: the high-volume exercisers tended to have a lower amount of mixed plaques and more calcified plaques.
Here are a few more studies on the relationship between exercise and CACS.
A study published in 2017 found that male masters endurance athletes had a higher prevalence of elevated CACS and coronary plaques, but most of these plaques were calcified. The control group was more likely to have plaques that were of a mixed morphology.
A 2020 study found that the total volume of exercise was not related to the progression of CACS in middle-aged male and female endurance athletes.
A study published in 2021 including over 25,000 healthy adult men and women found that those who engaged in higher levels of physical activity were more likely to have a CACS above zero and a worse CACS progression compared to the least-active group.
It is pretty clear that athletes often show higher CACS compared to control groups, despite the fact that they have better levels of other cardiometabolic risk factors such as body weight, blood pressure, and blood lipids.
This is concerning because higher CACS are associated with a greater risk for adverse cardiovascular outcomes. Engaging in physical activity does appear to lessen the risk associated with a higher CACS, but it doesn’t eliminate it! If you take two people with the same amount of coronary artery calcification, the more physically active person will be at a lower cardiovascular risk, however, both individuals will have a higher risk than someone with a low CACS.
Clearly, it’s important to consider your own health history, genetic risk for heart disease, cardiovascular risk factors, and symptoms when determining a safe level and intensity of exercise.
The good news is that athletes can follow some guidelines and take action. If you’re anything like me, this evidence is mildly concerning. I want to engage in high-volume exercise for the rest of my life, but not if it comes with a substantial health risk. Can we have our cake and eat it too?
In a recent editorial published in the British Journal of Sports Medicine, experts provide some advice and considerations for the athlete.